On August 25, 2016, the Washoe County Health District in Reno, Nevada, was notified of a patient at an acute care hospital with carbapenem-resistant Enterobacteriaceae (CRE) that was resistant to all (26) available antimicrobial drugs. The patient was a female Washoe County resident in her 70s who had recently arrived back to the United States after an extended visit to India. The patient developed septic shock and died in early September.
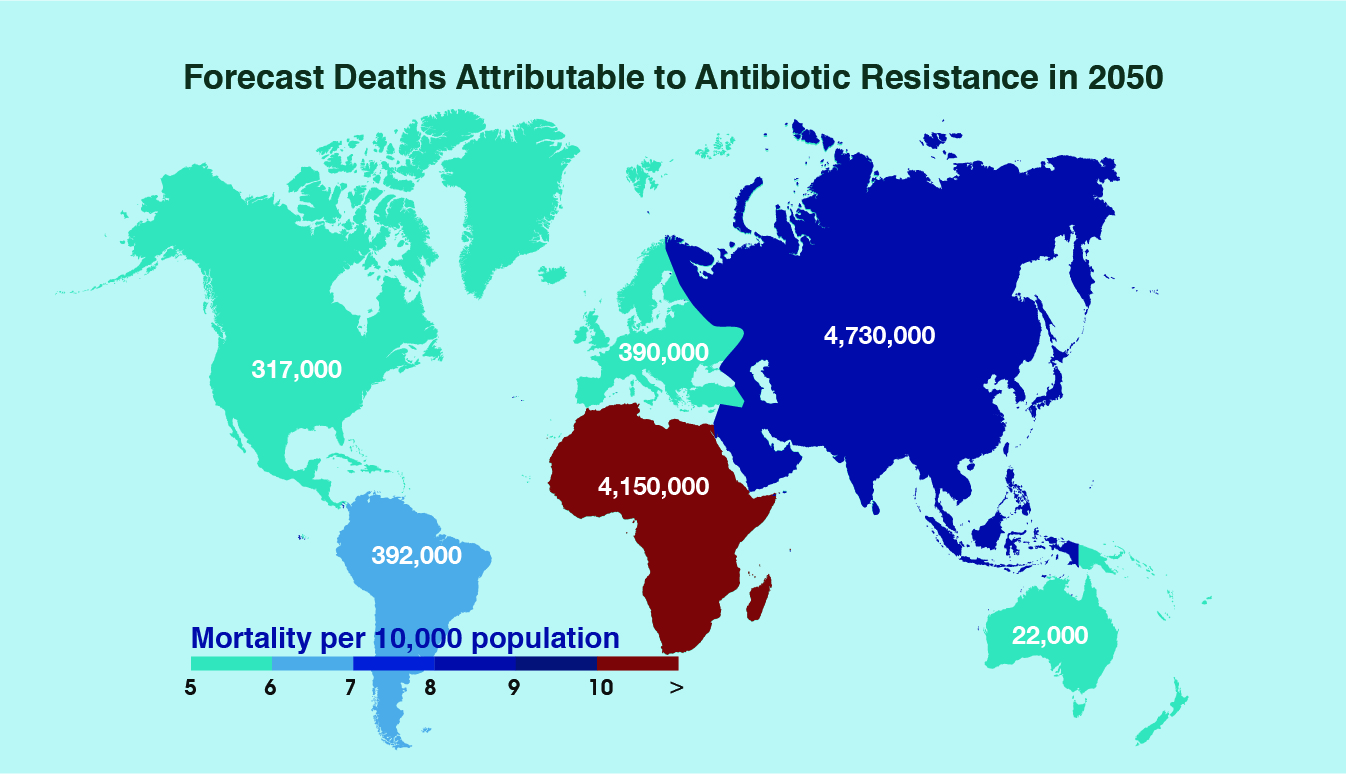
One of the greatest threats to global health today, antimicrobial resistance causes 700,000 deaths per year by comprising the effective prevention and treatment of an ever increasing range of infections. By 2050, this growing epidemic is expected to cause 10 million deaths annually and cost the world $100 trillion in lost economic output. Antimicrobial resistance has evolved to a point where we rely on only one or two antimicrobials in many parts of the world to fight our most severe infections and conditions, a dangerous, unsustainable precedent.
.
Source: Primal Group (2016)
.
For the first time ever, the World Health Organization published a list of antimicrobial-resistant ‘priority pathogens’ – a selection of 12 bacteria that pose the most significant threat to human health. The list has three rankings – critical, high and medium – according to how urgently new antimicrobials are needed. These include Acinetobacter, Pseudomonas and various Enterobacteriaceae that can cause severe and often deadly infections such as pneumonia and septicaemia. Top of the list are gut bacteria such as Escherichia coli – a deadly threat in hospitals around the world.
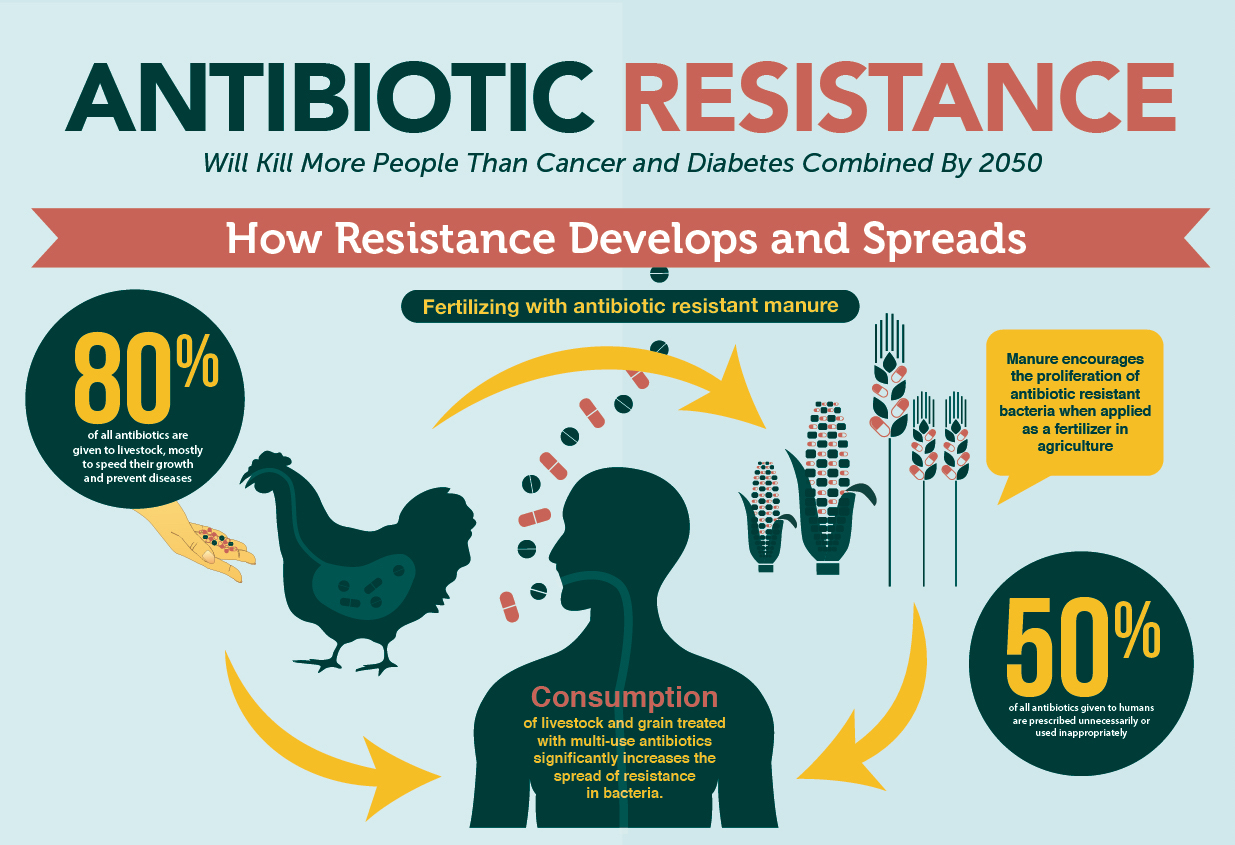
What has caused such a profound rise of antimicrobial resistance? Mainly negligence. The misuse of antimicrobial agents in healthcare is one of the main factors responsible. The US Centers for Disease Control and Prevention consider that 30% of the antibiotics prescribed today to treat a range of common infections are unnecessary. According to Nature, the average child in America is given 10-20 courses of antibiotics by the time he or she reaches adulthood. That’s on average one dose every two years! The other culprit of antibiotics overuse is in agriculture. 80% of the 150,000 metric tons of antibiotics produced each year in the United States are used exclusively for promoting growth and health in livestock.
.
Source: Primal Group (2016)
.
We desperately need smart science, business and finance to solve antibiotic resistance. At the moment there is little financial incentive to develop more antimicrobials, for which there is an astounding need. Researchers at the Massachusetts Institute of Technology have engineered an antimicrobial peptide that can eliminate many types of bacteria, including some of the antimicrobial resistance superbugs mentioned above, through new and improved CRISPR technology. On the political front, China has banned antibiotics as an animal feed additive and the European Union has recommended that use in agriculture be slashed by two thirds. Many of the world’s largest food producers, such as Wal-Mart, Tyson Foods and McDonalds, are committing to sell only antibiotic free produce.
Even so, such moves from the world’s foremost commercial organizations and scientific institutions take considerable time. We must therefore reduce the unnecessary use of antimicrobials and utilize them more sparingly.
Adopting ecological alternatives for antimicrobial use in agriculture is showing considerable promise. Natural additives for livestock feed such as neem cake are gaining popularity in farms worldwide. With the ability to eradicate microbes that cause infections and disease in livestock, neem fights bacteria, preventing illness in livestock, and alleviating the pressure of rising antimicrobial resistance. With an ample amount of essential nutrients like protein, calcium, carotene and a host of other minerals required for healthy growth in livestock, neem is a cost-effective and promising alternative to the overuse of antimicrobials in agriculture.