“This may be the most important year for Antimicrobial Resistance that we’ve had in our lifetime.”
Keiji Fukada – Assistant Director General of the World Health Organization, May 2016
One of the most significant threats to mankind now and in the coming decades, infectious microbes around the world continue to develop resistance to many of our most effective antibiotics. As we continue to proliferate the use of these drugs across agriculture and healthcare we incur a greater risk of reverting to the dark ages of medicine where the most common treatments and infections become potentially deadly.
700,000 people are killed every year due to drug-resistant infections, a death toll that, if left unabated, is expected to increase dramatically to 10 million by 2050. Antibiotic resistance has evolved to a point where we rely on one or two antibiotics in many parts of the world to fight our most severe infections and conditions. Surprisingly, it is old infections (not new ones) that need to be most feared. From typhoid to clostridium difficille, these old pathogens are becoming killers once again.
What has caused this rise of antimicrobial resistance? Negligence. Those responsible are not aware of the true consequences of their actions, which are affecting society as a whole. The UK Review on Antimicrobial Resistance deems over half of all antibiotics prescribed in medicine today as unnecessary. The proliferation of antibiotic use is even more severe in agriculture. In the United States, more than 70% of antibiotics are used for agriculture and the majority of these drugs are considered as ‘last resort’ treatments across global healthcare.
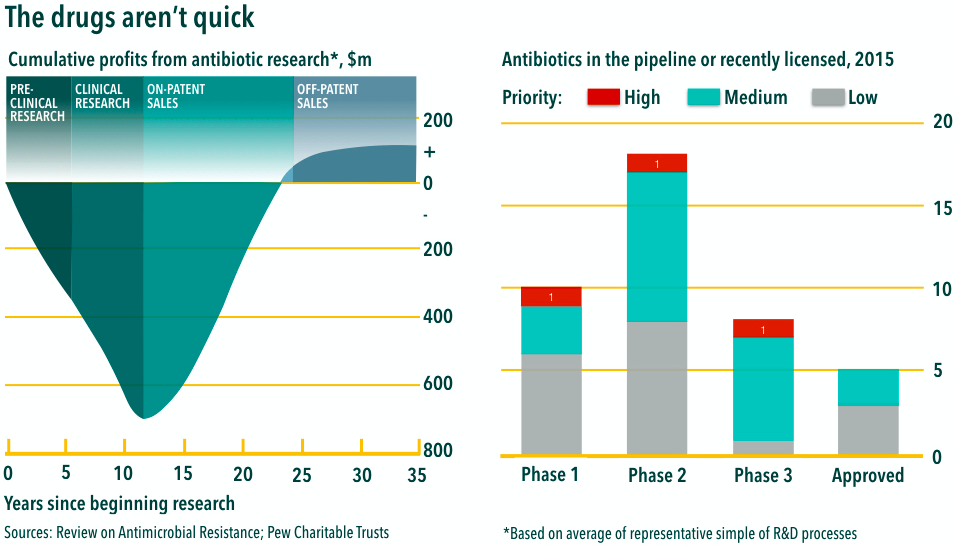
We desperately need smart science and economics to solve our supply problem. At the moment there is little financial incentive to develop more antibiotics for which there is an astounding need. Pharmaceutical companies are not interested in creating new drugs as its development cycle represents a huge investment with little payoff. Less than 5% of venture capital investment in pharmaceutical Research & Development between 2003 and 2013 was for antimicrobial development. A mere 40 products are currently receiving clinical trials and only a fraction of these drugs will ever reach the market.
We must therefore reduce the demand for antibiotics and utilize them more sparingly. Knowing your enemy through rapid diagnostic systems would effectively transform the way we use antimicrobials in humans and animals. Improving hygiene across agriculture and healthcare is another effective method. A fundamental first step would be to significantly reduce antibiotic use in agriculture through globally agreed targets and restrictions on certain type of critical drugs. The European Union has taken the lead in accepting this responsibility and has agreed to ban the use of antibiotics necessary for human health in livestock agriculture.
Adopting ecological alternatives for antibiotics use in agriculture is showing considerable promise. Natural additives for livestock feed such as neem cake are gaining popularity in farms worldwide. Containing essential nutrients such as protein, calcium and carotene required for healthy growth in livestock, with the ability to eradicate microbes that cause infections and disease, neem helps to fight bacteria and alleviates the pressure of rising antibiotic resistance.
We need a multi-faceted approach in order to transform the way we utilize antimicrobials around the world. The solutions must work for as many people as possible, be cost effective and support economic development. Although a significant challenge, we are well within our ability to solve this rise of antibiotic resistance.