In a declaration of defeat, the World Health Organization (WHO) no longer considers Zika a Public Health Emergency of International Concern. Although this may seem like good news, this decision in fact reflects the severity of Zika’s rapid transition from obscurity to a permanent threat to human health. The disease now joins the ranks of HIV, XDR-TB, Ebola, Marbug, Dengue and an exhaustive list of other killers that have spread around the world in record time.
The escalation in severity has been remarkable. First documented nearly seventy years ago, Zika was originally considered harmless. 80% of those originally infected demonstrated no physical symptoms. This changed drastically over the past year when the first cases of microcephaly and Guillain-Barre syndrome began to appear.
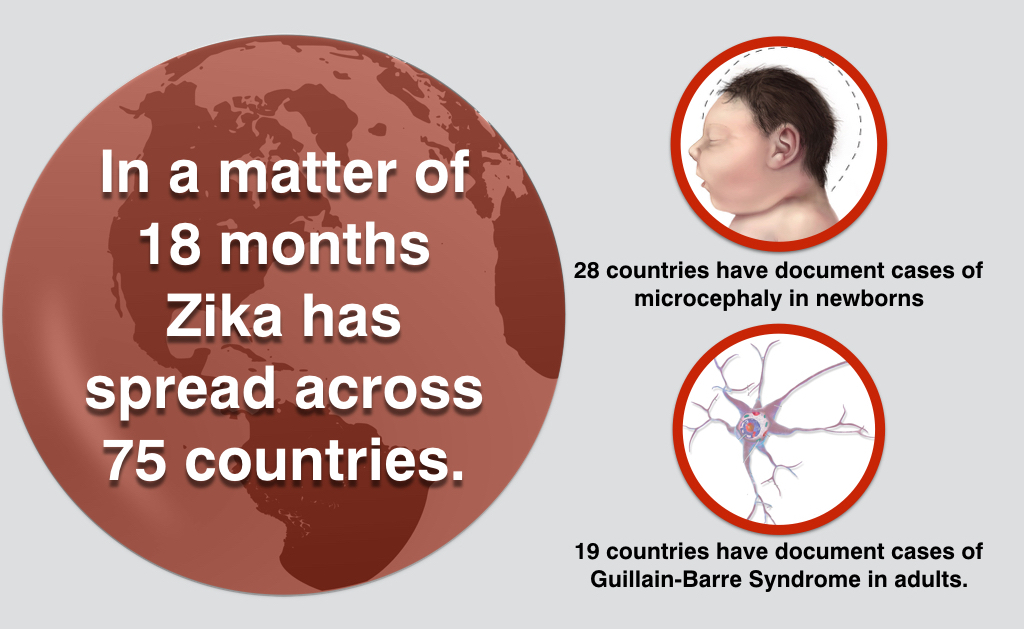
In a matter of 18 months Zika has spread across 75 countries. Among them, 28 have document cases of microcephaly, the severe brain damage deformation caused by viral infection of the fetus. 19 have had cases of Guillain-Barre Syndrome, a form of paralysis seen in infected adults. The WHO still expects an increase in infections around the world and they are unable to predict at what incidence rate. The virus has now entered a phase that required a longer-term response mechanism and sustained resources.
Scientists and Physicians at the WHO claim the reason for removing the emergency status was the profound mystery surrounding Zika. There is no treatment, cure, reliable in utero diagnostic or vaccine for the virus at this time. Tom Frieden, Head of the Centers for Disease Control and Prevention (CDC), declared that ‘Zika is not controllable’.
Zika and its complications are here to stay. Healthcare facilities around the world are engaged in an all-out race to slow the spread of Zika. Never before have so many organizations and governments worked so quickly to create a vaccine, although don’t hold your breath as the average development time for these drugs is well over a decade. After significant debate, the Obama administration approved $1.1 billion in funding the fight against Zika and at least $400 million of this will be dedicated to crating vaccines and an effective diagnostic testing system. Although we have no point-of-care diagnostic and recuperative tool for Zika, we can in fact protect ourselves through repellency methods against the virus’ carrier mosquito Aedes Aegypti.
Aedes aegypti, the yellow fever mosquito, can also spread dengue fever, chikungunya, malaria and yellow fever viruses and a variety of other diseases, which together affect up to 200 million people every single year.

A powerful, effective and non-toxic pesticide, neem has evolved from being a ‘traditional’ medicine and alternative in crop core to the subject of studies showing its effectiveness in reducing the transmission of mosquito-borne diseases.
With anti-feedancy, fecundity suppression, ovicidal and larvidical activity, growth regulation and repellence against 600 different insect species (including Aedes Aegypti, neem rarely induces resistance. A study by the Massachusetts Institute of Technology shows how neem seeds, dried, ground into a coarse powder and then sprinkled onto known mosquito larvae breeding grounds resulted in 49% fewer adult females. As the study pointed out, targeting the larval phase of mosquitoes is cost effective with minimal environmental impact.
Entirely biodegradable, efficient and cost effective, organic insecticides such as neem are valuable solutions to this public health issue.